Psoriasis
About Psoriasis
Psoriasis is a chronic skin disorder that causes red, scaly patches on the limbs, trunk, scalp, and other parts of the body. It is not contagious. The rash of psoriasis goes through cycles of improving and worsening. A period of worsening is called a "flare". At times, psoriasis can be disfiguring, uncomfortable, and even painful. The scaling and unpleasant appearance of psoriasis lesions (especially if left untreated) can cause embarrassment and be a significant source of anxiety or depression. About 10-30% of people with psoriasis will also develop psoriatic arthritis. Symptoms of psoriatic arthritis include stiffness, pain, and swelling of the tendons and joints, as well as morning stiffness and generalized fatigue.
Treatment Options
Topical corticosteroids are often the first line treatment in Psoriasis. Corticosteroids play an important role in controlling the body’s inflammatory response. Researchers think that in patients with psoriasis, the body’s immune system attacks its own skin cells resulting in redness, scaling, and swelling. Topical corticosteroids exert an anti-inflammatory effect on the skin and can help heal psoriasis plaques. Topical corticosteroids come in a variety of potencies ranging from mild over the counter creams to more potent prescription ointments. Milder over the counter creams are often reserved for areas of thin skin such as the face while potent prescription ointments are used for thick skin areas such as the elbows and knees. For patients that dislike ointments, corticosteroid foams and gels are available.
Topical vitamin D (calcipotriene) is a synthetic vitamin D3 derivative formulated to slow growth of skin cells, flatten lesions and remove scales. Although topical vitamin D can be used alone, better results are often observed in combination with topical corticosteroids. Topical vitamin D is best used in a limited amount to reduce side effects. Topical vitamin D (calcipotriene) is available as a cream, solution, ointment, or foam.
Phototherapy is beneficial for the control of psoriatic skin lesions. UV radiation is thought to have anti-inflammatory and antiproliferative effects on skin cells. Regular exposure of the skin to UV light under medical supervision is a safe an effective means of controlling psoriasis. Home phototherapy is available in select patients, but can be expensive. Tanning beds predominately use a type of light (UVA) that is not as helpful for managing psoriasis. Photochemotherapy (PUVA) involves treatment with a photosensitising agent called psoralen either by pill or bath, then administering UV light under the supervision of a dermatologist. Excimer laser can be used on small psoriasis plaques with excellent results. By using a narrow beam, comparably high doses of UV light can be administered to focal psoriasis plaques. Some studies suggest laser therapy can result in faster response than conventional phototherapy.
Non-Biologic Systemics are a class of medications taken orally that act systemically on the immune system. Methotrexate has been used successfully to treat psoriasis for over 30 years. It also effective in psoriatic arthritis and psoriatic nail disease. In patients with psoriasis, immune cells called T cells attack the skin resulting in excessive growth of skin cells. Methotrexate inhibits DNA synthesis in these immune cells, thus reducing inflammation and controlling psoriasis plaque formation. Due to its relatively inexpensive cost, methotrexate is usually attempted before starting biologic therapy. Apremilast (Otezla) is a new oral medication that inhibits the enzyme phosphodiesterase 4. Inhibition of this regulatory protein results in decreased downstream release of the inflammatory protein TNF-α, which has shown to be implicated in psoriasis. Apremilast therefore has many of the advantages of traditional biologics such as decresed levels of the inflammatory protein TNF-α with the convienence of oral administration. Apremilast is FDA approved for both plaque psoriasis and psoriatic arthritis.
Biologic Systemics are a class of medications taken by injection that act systemically on the immune system. Biologic systemics differ from traditional non-biologic systemic immune suppressing drugs such as methotrexate in that they only affect specific targets in the immune system instead of causing wide spread effects. TNF-α Blockers are a class of biologic medications that act on TNF-α, a protein in the body which initiates the inflammatory cycle implicated with psoriasis. These drugs include Enbrel, Stelara, Remicade and Humira among a variety of other TNF-α blockers. Typically these drugs are used for patients with a history of treatment failure with traditional therapy or people who also have psoriatic arthritis associated with their condition. Both psoriasis and psoriatic arthritis are marked by excess production of the cytokine TNF-α in both the skin and joints which causes rapid growth of affected skin cells as well as damage to joint tissue. The blockade of the production of TNF-α by these biologic drugs prevents the inflammatory cycle caused by this cytokine and helps treat the manifestations of psoriasis and psoriatic arthritis Ustekinumab (Stelara) is a human monoclonal antibody that binds inflammatory proteins IL-12 and IL-23. These two proteins play an important role in the body's inflammatory response in psoriasis. In general, monoclonal antibodys are biologic proteins that bind other proteins within the body. In the case of Ustekinumab, this protein based drug binds inflammatory proteins IL-12 and IL-23, thus reducing the inflammatory response to help improve psoriasis plaques. Ustekinumab is FDA approved for treatment of plaque psoriasis and psoriatic arthritis. Some recent studies suggest it may be more effective than TNF-α blockers. Secukinumab (Cosentyx) is a human monoclonal antibody that binds inflamatory protein IL-17. This protein is also thought to play a role in the body's inflammatory response in psoriasis. Recent studies suggest Secukinumab may be more effective than TNF-α blockers. Secukinumab is FDA approved for moderate to severe plaque psoriasis.
Treatment Side Effects
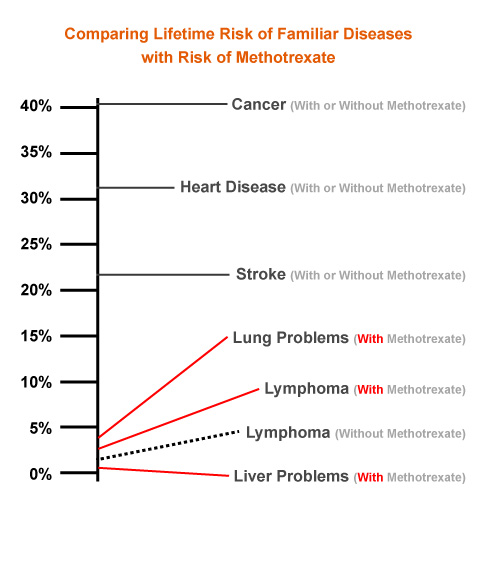
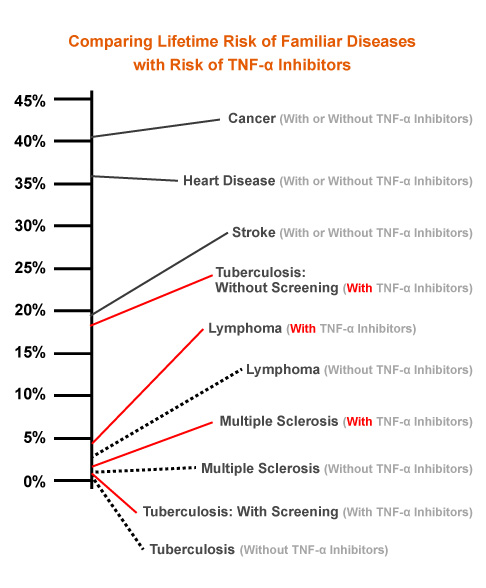
Topical Corticosteroids High potency corticosteroids do carry some risks of side effects such as skin thinning, pigment changes, increased bruising, redness, stretch marks and dilation of the superficial blood vessels. Side effects can be reduced by alternating with other non-corticosteroid topical agents such as Topical Vitamin D. Topical Vitamin D The most common side effects of topical vitamin D are skin irritation, stinging, and burning. Light Therapy The most common side effect of phototherapy is redness and blistering. The use of a skin moisturizer may be used to reduce side effects which include redness and itchy, dry skin. When using phototherapy, it is important to consider the potential for UV radiation to accelerate photodamage and increase the risk of skin cancer. Non-Biologic Systemics Methotrexate's long-term side effects include liver damage and reversible liver scarring (especially in patients who drink alcohol) and rarely certain cancers such as lymphoma and bone marrow toxicity. Folic acid, 1 mg daily, can protect against some side effects. Patients on methotrexate must undergo regular blood tests and have liver biopsies at set intervals to make sure the drug is not harming the liver, white blood cells or bone marrow. Apremilast (Otezla) is considered a safe and effective medication. Common side effects include headache, nausea, fatigue. In rare cases there have been reports of depression and mild weight loss. Biologic Systemics Biologics generally have excellent efficacy and tolerability, but must still be used with caution as they can have negative immune system effects and may permit life-threatening infections to take place. Tuberculosis screening must be performed in all patients taking these medications to prevent life-threatening complications. For a graphical representation of these risks, please see the chart below.